Estrogen-related receptors, or ERRs, are a family of “orphan” nuclear receptors discovered in the late 1980s. Despite their name, ERRs do not bind estrogen. Instead, they act like switches to turn on genes that control our cells’ energy use. ERRs belong to the nuclear receptor family of proteins (similar to hormone receptors) but have no known natural hormone that activates them. Because of this, scientists originally couldn’t “turn them off” with a hormone, so they were called “orphan” receptors. Researchers later realized ERRs are ancient regulators of energy: as one review notes, ERRs occupy “a strategic node” in controlling cellular energy metabolism and are “central regulators of energy homeostasis”. In plain terms, ERRs are master energy managers for the body. They are especially active in high-energy tissues – skeletal muscle, heart, brain and brown fat – where they help control fuel-burning processes. Some scientists even prefer to call them “energy-related receptors” instead of estrogen-related.
ERRs were first cloned by Ronald Evans and colleagues, who noted their strong similarity to estrogen receptors. Evans later remarked that discovering ERRs was like finding “molecular gold” in understanding animal evolution. For over three decades researchers have been peeling back their role. Now we know that, unlike classic estrogen receptors, these receptors constantly (and constitutively) stimulate genes for metabolism. For example, they directly control many genes for glucose breakdown, fat burning, and mitochondrial function. In fact, ERRs work closely with important “fuel sensors” like PGC-1α (a protein that tells cells to make more mitochondria). The result is that ERR act like gas pedals for our cellular engines: when ERRs are active, cells build more mitochondria and crank up energy production.
Estrogen-related receptors in Metabolism and Muscle Function
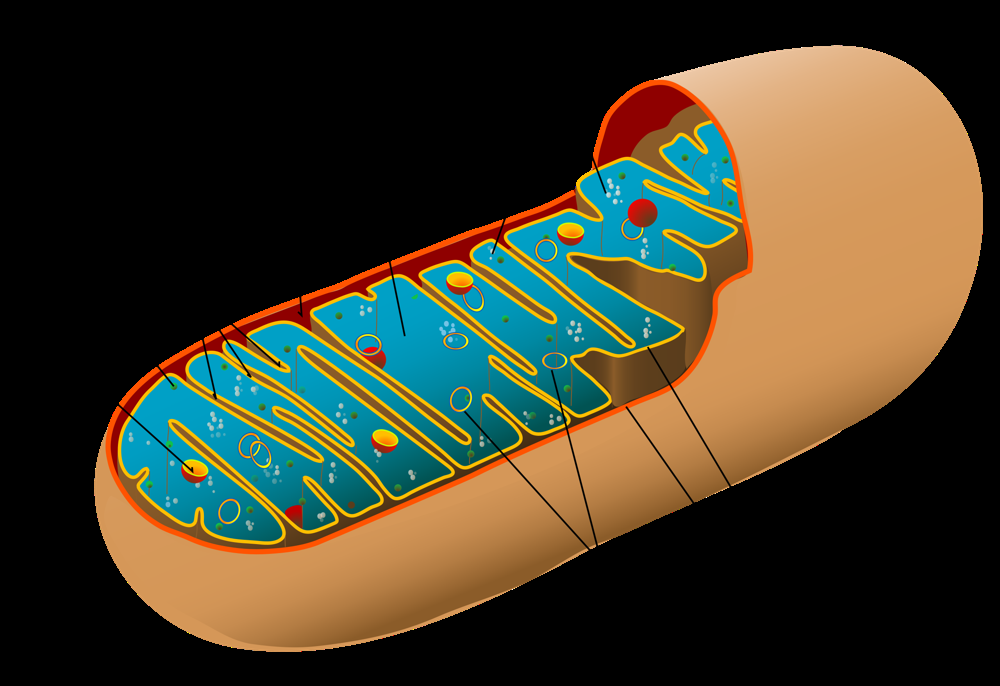
Cells rely on mitochondria – the “powerhouses” of the cell – to convert food and oxygen into usable energy. ERRs play a critical role in managing these powerhouses. In muscle cells, for instance, ERRs help build new mitochondria and keep them running efficiently. Studies in mice show this clearly: mice engineered to lack both major muscle ERRs (ERRα and ERRγ) become severely exercise-intolerant, even though they are otherwise healthy. These mice cannot sustain normal running or weightlifting because their muscles cannot produce enough energy. By contrast, when ERRs are present and active, muscles respond well to exercise. ERRα/γ help muscles adapt to workouts by “turning on” hundreds of genes for oxidative metabolism. In one recent study, researchers found that after exercise training, ERRα and ERRγ are essential for the surge in mitochondrial production. As Ronald Evans summarized, ERRs turned out to be “indispensable drivers of mitochondrial growth and activity in our muscles,” making them a promising target for treating muscle fatigue and weakness.
ERRs also influence metabolism beyond muscle. In the liver and fat tissue, ERRs help regulate blood sugar and fat storage. For example, ERRα suppresses glucose production in the liver and boosts fat burning. This means activating ERRα makes the liver send out less sugar and burn more fat – both helpful for blood sugar control in diabetes. Conversely, scientists have observed that removing ERRα entirely can have mixed effects. In one mouse study, knocking out (deleting) ERRα in all tissues actually protected mice from obesity on a high-fat diet. These mice burned fat faster and absorbed less fat. That surprising result shows the biology is complex: ERRs have slightly different roles in different tissues. But overall, ERRs are considered major controllers of energy balance. They sit in the genome right next to genes for glycolysis, fat metabolism, and the electron transport chain.
In healthy muscle, ERRs respond to signals like exercise, fasting or cold to ramp up metabolism. In fact, a 2023 review notes that normal metabolic stress (exercise, diet) increases ERR activity in muscle, whereas conditions like diabetes or muscular dystrophy suppress ERR expression. This suggests that disease states may turn down this energy switch, contributing to muscle weakness and metabolic problems.
Recent Research Highlights
- Exercise-mimicking drugs for obesity/diabetes. A 2024 study tested an experimental compound called SLU-PP-332 that activates all ERRs like an “exercise pill”. In obese mice, SLU-PP-332 triggered many of the same benefits as exercise. The treated mice burned more energy and fat, gained less weight, and became more sensitive to insulin. In other words, the drug reduced obesity and improved insulin resistance in mice models of metabolic syndrome. The authors conclude that pharmacologically activating ERRs “may be an effective method to treat metabolic syndrome and obesity”. As Dr. Thomas Burris (co-author) noted, ERR agonists could become a “potential new class of drugs” for type 2 diabetes and obesity.
- Boosting muscle mitochondria in degenerative muscle disorders. In May 2025, a Salk Institute team reported in PNAS how ERRα and ERRγ cooperatively control muscle energy. They showed that these receptors are essential for muscles to make more mitochondria when needed. Importantly, they found that developing drugs to boost ERR activity in muscle could help diseases where muscles lack energy. A press release summarized that “a drug to boost ERRs could be a powerful way to restore energy supplies in people with metabolic disorders, such as muscular dystrophy”. In short, activating ERRs in muscle may help patients with muscle-wasting diseases or age-related weakness by recharging the muscle “batteries”.
- Liver and systemic metabolism studies. Other recent work highlights ERRα in liver and fat. ERRα normally downregulates gluconeogenesis (glucose-making) and upregulates fat oxidation. Studies in animal models show that higher ERRα activity goes hand-in-hand with better insulin sensitivity, whereas low ERRα is linked to fatty liver and diabetes. For example, researchers found that in insulin-resistant patients, the genes controlled by ERRα are often turned down in muscle, and higher ERRα levels correlate with better insulin sensitivity. In lab and animal studies, plant compounds like genistein (found in soy) that activate ERRα have shown benefits: they improve fatty liver and increase fat burning in mice, and even showed promise in early human trials for fatty liver disease.
- Protecting the heart and aging muscle. ERRs are also being explored for heart health and sarcopenia. In older mice, ERR levels naturally decline, which may contribute to age-related muscle loss. Dr. Burris notes that ERR agonists might even combat “muscle weakness in the elderly”. In heart studies (in animals), activating ERRs helped protect against heart failure by keeping the heart’s energy metabolism robust. These findings suggest ERR-targeted therapies could have broad uses across metabolic and muscle aging conditions, although clinical proof in people is still pending.
Looking Ahead: Estrogen-related receptors-Targeted Therapies
Scientists are now actively pursuing ERR-based treatments. One approach is to develop small molecules (drugs) that specifically activate ERRα, ERRγ, or both. The success of SLU-PP-332 in mice suggests “exercise-mimetic” pills are possible. Researchers envision drugs that could, for example, mimic exercise, boost fat burning, or stimulate muscle mitochondria to fight wasting. Dr. Burris describes ERR agonists as tapping into “natural pathways that are stimulated during exercise”.
Another avenue is nutritional or supplement strategies. Since compounds like genistein can activate ERRα, there is interest in dietary ERR activators. Indeed, genistein has been shown to raise ERRα activity, increase energy expenditure, and improve fatty liver in rodents. Clinical trials of genistein for nonalcoholic fatty liver disease have shown safety and some benefit, hinting that modulating ERRs through diet might be feasible.
Researchers are also thinking about precision targeting. ERRs have different roles in muscle, liver, and fat, so the ideal drug might activate ERRs in one tissue (like muscle) without causing unwanted effects elsewhere. Some reviews suggest the future may see tissue-specific ERR modulators. For example, a muscle-specific ERR activator could boost endurance without affecting fat storage.
Of course, caution is warranted. The biology of ERRs is complex. We’ve seen that completely removing ERRα in mice can sometimes protect against weight gain, while in other situations ERRα activity is beneficial. Future therapies will need to balance these effects. Ongoing research aims to answer key questions: Are these drugs safe in the long term? Do they work in humans as they do in mice? Which patient groups will benefit most? Early evidence is promising, and ERRs now stand out as a “promising target” for treating metabolic and muscle diseases.
In the next few years, clinical trials may begin to test ERR-targeting compounds. If successful, we could have new tools to combat obesity, diabetes, muscle wasting and more – all by harnessing the power of these once-mysterious energy-related receptors.